As an epidemiologist, I’d be remiss if I didn’t raise a little awareness about health concerns starting to wedge into our everyday lives. Don’t worry. It’s not a threat countdown. Think of it as your friendly nerdy gal pal saying, “Heads up. Know these names, not because it’s a dire emergency, but because awareness is your best line of defense.”
1. Chagas Disease (“Kissing Bug” Disease)
Cause: Chagas disease is caused by the parasite Trypanosoma cruzi, a microscopic protozoan.
Transmission:
- The parasite is spread primarily by triatomine insects, often called “kissing bugs” because they tend to bite humans around the mouth or eyes at night.
- Infection occurs when the insect’s feces, which contain the parasite, are accidentally rubbed into the bite wound, eyes, or mouth.
Early Phase:
- Most people do not show symptoms right after infection.
- If symptoms do appear, they may include: fever, fatigue, swelling at the bite site (called a “chagoma”), or swelling of the eyelid (called “Romaña’s sign”).
Long-Term Risks:
- The danger comes years later. Without treatment, the infection can become chronic, leading to:
- Heart disease (arrhythmias, heart failure, sudden cardiac arrest)
- Digestive complications (enlarged esophagus or colon, causing swallowing or bowel problems)
Geographic Spread in the U.S.:
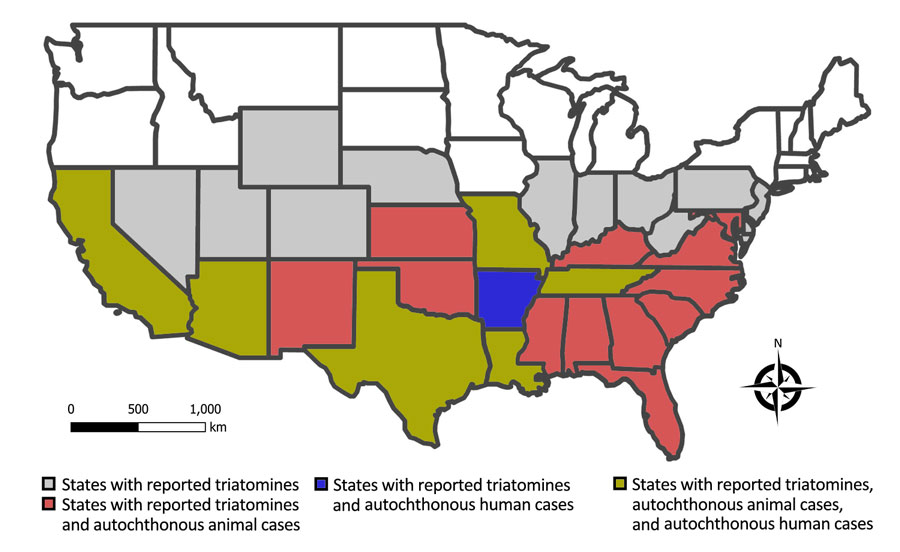
- Locally acquired human cases (not travel-related) have been confirmed in Arizona, Arkansas, California, Louisiana, Mississippi, Missouri, Tennessee, and Texas.
- Triatomine bugs themselves are now known to exist in 32 U.S. states, meaning the potential for exposure is more widespread than many realize.
Why It Matters: most U.S. cases are still linked to Latin America, but the presence of the bug across much of the country and confirmed local transmission highlight the need for awareness.
Protective steps:
- Seal cracks and use insect screens.
- Use repellent and avoid bug travel.
- Get tested, if exposed.
2. Babesiosis (buh-BEE-zee-oh-sis) Disease
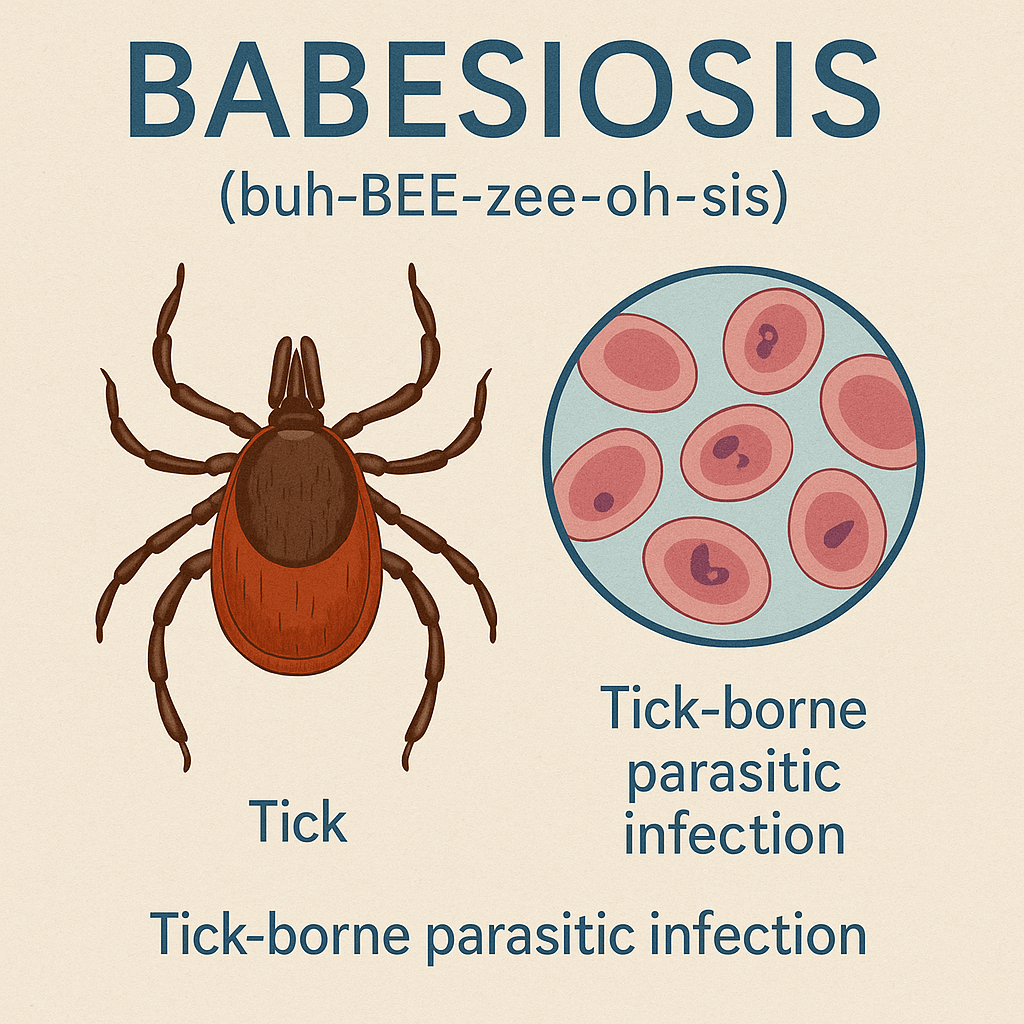
Cause:
- Caused by Babesia parasites, microscopic single-celled organisms that infect red blood cells.
- They are similar to malaria parasites in appearance and behavior.
Transmission:
- Spread through the bite of infected black-legged ticks (Ixodes scapularis): the same tick that transmits Lyme disease.
- Less commonly, babesiosis can be transmitted through blood transfusions or from mother to baby during pregnancy.
Early Symptoms:
- Many cases are silent, especially in healthy individuals.
- When symptoms occur, they usually appear 1–6 weeks after a tick bite and include: Fever, Chills, Headache, Body aches, Fatigue
Complications: can be severe, particularly in older adults, immunocompromised people, or those without a spleen.
- May cause:
- Very low red blood cell counts (hemolytic anemia)
- Difficulty breathing
- Low blood pressure
- Organ failure (kidney or liver)
Areas of Concern in the U.S.:
- Most common in the Northeastern and upper Midwestern states, including: Massachusetts, Rhode Island, Connecticut, New York, New Jersey, Pennsylvania, Vermont, New Hampshire, Maine, Minnesota, Wisconsin.
- Clusters of cases also detected in Indiana, Kentucky, Missouri, Tennessee, and Virginia.
Why It Matters: cases are rising in the U.S., with the disease now considered endemic in multiple states. Because many infections are silent, it can spread unknowingly through blood transfusion.
Protective steps:
- Wear long clothing and treat with repellent.
- Check for ticks carefully after outdoor activities.
3. New World Screwworm Larvae Infection
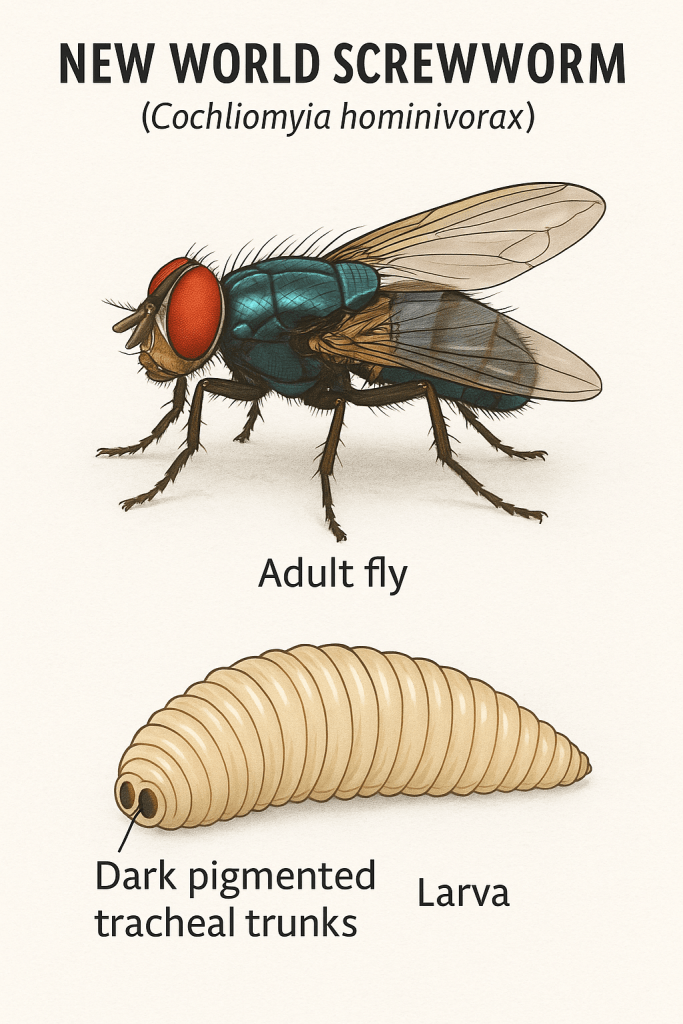
Cause: larvae of the New World screwworm fly, which feed on living tissue (unlike most maggots that feed on dead tissue).
Transmission:
- Female flies lay eggs in open wounds or natural body openings of animals and humans.
- Hatched larvae burrow into healthy tissue, enlarging wounds and causing rapid destruction.
Symptoms:
- Humans/animals: severe pain, foul-smelling wounds, visible larvae (“worms”) moving in a screw-like motion.
- Can lead to infection, disfigurement, and even death, if untreated.
Impact:
- Major economic threat to livestock (cattle, sheep, goats, horses, pigs, deer).
- Human cases are less common, but serious.
Geography:
- Once widespread in the Americas; eradicated from the U.S. and Central America through the Sterile Insect Technique (SIT).
- Still endemic in South America and some Caribbean regions; reintroductions remain a threat (e.g., Florida Keys outbreak in 2016).
Treatment & Control:
- Prevention depends on surveillance and continued sterile insect release programs.
- Immediate removal of larvae and wound care.
- In livestock, ivermectin may be used.
Protective steps:
- Seek urgent care for unusual wounds, especially after travel.
- Animal and livestock monitoring remain critical.
4. Candida auris Fungal Infection
Cause: the fungus Candida auris, an emerging multidrug-resistant yeast that spreads easily in healthcare settings.
Transmission:
- Moves from person to person or via contaminated surfaces/equipment.
- Can silently colonize the skin, making outbreaks difficult to detect.
Symptoms:
- Often causes invasive infections in the bloodstream, wounds, or ears.
- Symptoms mimic bacterial sepsis (fever, chills) and can be easily misdiagnosed.
Impact:
- High mortality (30–60%) in vulnerable patients.
- Many strains are resistant to multiple antifungals; some to all three major drug classes.
- Requires strict infection-control to prevent rapid spread in hospitals and nursing homes.
Geography:
- First identified in 2009 in Japan.
- By 2025, confirmed in over 40 countries and across much of the U.S., with outbreaks reported in New York, New Jersey, Illinois, California, Florida, Texas, Nevada, and beyond.
- U.S. cases have risen sharply, more than tripling between 2019–2022, and continuing upward into 2025.
Why It Matters in 2025:
- Still designated a global urgent health threat by CDC and WHO.
- Rising case counts and expanding outbreaks.
- Increasing reports of pan-resistant strains with no reliable treatment.
- Silent colonization makes containment difficult.
Protective steps:
- For healthcare settings: strict infection control and early detection.
- For individuals at high risk: confirm environment safety and personal hygiene.
Conclusion: Awareness as Prevention
Chagas, Babesiosis, New World Screwworm, and Candida auris aren’t dinner-table topics in the U.S., but they’re not science fiction either. They remind us that in a connected world, health threats don’t stop at borders.
The aim here isn’t alarm, but awareness. While the overall risk to most people is low, these infections and infestations highlight how vigilance and everyday practices (i.e., using insect repellent, caring for wounds properly, maintaining good hygiene, and paying attention to public health updates), can make a real difference.
Think of this knowledge as a toolkit, not a warning bell. The more familiar we are with emerging names and patterns, the better equipped we are to recognize problems early, ask the right questions, and strengthen community health—which is, ultimately, the goal.
References (APA)
Centers for Disease Control and Prevention. (2024). Chagas disease in the United States. Emerging Infectious Diseases, 31(9), Table and Figure. https://wwwnc.cdc.gov/eid/article/31/9/24-1700_article
Centers for Disease Control and Prevention. (2025, August 26). Travel-associated New World screwworm case confirmed; prevention measures in place. CDC.gov. https://www.usda.gov/…
Centers for Disease Control and Prevention. (2023, MMWR Reports). Trends in Reported Babesiosis Cases — United States. https://www.cdc.gov/mmwr/…
Centers for Disease Control and Prevention. (2025, March 20). * Candida auris rises as urgent threat*. CDC.gov. https://www.cdc.gov/media/releases/2023/p0320-cauris.html
Centers for Disease Control and Prevention. (2025, August 28). Melioidosis caused by Burkholderia pseudomallei—Clinical overview and environmental findings. CDC.gov. https://www.cdc.gov/melioidosis/hcp/clinical-overview/index.html
People. (2025, September). Deadly ‘Kissing Bug’ Disease Chagas Has Spread in the U.S.—Which States Are Affected. People Magazine. https://people.com/deadly-kissing-bug-disease-chagas-has-spread-in-us-states-affected-11804956
Soucheray, M. (2024, October 8). Babesiosis rates rising steadily in the U.S. CIDRAP. https://www.cidrap.umn.edu/tick-borne-disease/babesiosis-rates-rising-steadily-us

